Imbalanced Nutrition Nursing Care Plan for Senior Wellness
Maintaining good nutrition in senior living is not always simple. With age, dietary needs change, and so do physical and emotional challenges that affect how well older adults eat. That’s why creating a comprehensive imbalanced nutrition nursing care plan is crucial to supporting residents’ overall health, independence, and quality of life.
This guide will explain the causes and assessment of nutritional imbalances, outline effective nursing strategies, and show how tailored plans can transform care outcomes. At NestBeyond, we believe in proactive care built on compassion, precision, and a deep understanding of every resident’s unique needs.
Understanding Imbalanced Nutrition in Senior Living
Imbalanced nutrition happens when the body doesn’t receive the right amount of nutrients to function properly. In senior living, this often occurs due to poor appetite, physical decline, chronic illnesses, and medication side effects. These factors can lead to malnutrition or overnutrition—both of which have serious consequences.
A proper, imbalanced nutrition nursing care plan begins with understanding these root causes. You may observe residents losing weight unexpectedly, suffering from fatigue, or showing changes in skin or muscle mass. These signs indicate that an imbalanced nutrition related to inadequate intake or poor absorption is present and must be addressed immediately.
Personalized interventions and good diet planning significantly prevent such issues and ensure seniors maintain vitality and joy throughout their golden years.
Common Causes of Nutritional Imbalance Among Seniors
Nutritional imbalances don’t just stem from food preferences. A mix of social, medical, and emotional factors often causes them. One of the most common issues seen in a nursing care plan for nutrition imbalance, less than body requirements, is low caloric or protein intake due to loss of appetite, difficulties swallowing, or limited access to nutritious meals.
Residents managing chronic conditions like diabetes or heart disease may have dietary restrictions that limit variety. These restrictions can exacerbate an imbalanced nutrition related to disease management, medication side effects, or even financial limitations that make it difficult to obtain high-quality meals.
Psychological challenges like depression or cognitive decline also affect food intake, making a thorough and compassionate assessment all the more essential. For an in-depth discussion, this article on elderly malnutrition provides excellent insights into what caregivers need to consider.
Nursing Assessment Techniques for Nutritional Status
Nurses must gather both subjective and objective data to create an effective imbalanced nutrition nursing care plan. This includes observing appetite patterns, evaluating food preferences, and reviewing weight trends over time. Objective measurements like BMI, lab results, and muscle tone analysis offer valuable insight into physical status.
During assessment, be alert to the patient’s mobility, cognition, and eating environment. These can all influence whether a resident is getting the nutrition they need. Using this data allows for a precise, imbalanced nutrition nursing diagnosis, which forms the foundation for further planning.
Engaging culinary teams, like those mentioned in this dietary guide for seniors, ensures meals align with health requirements and personal enjoyment.
Effective Nursing Interventions for Nutritional Improvement
Once a diagnosis is made, you can initiate imbalanced nutrition interventions tailored to the resident’s unique needs. These may include:
- Administering supplements for vitamins, minerals, or calories
- Encouraging nutrient-dense, frequent small meals and snacks
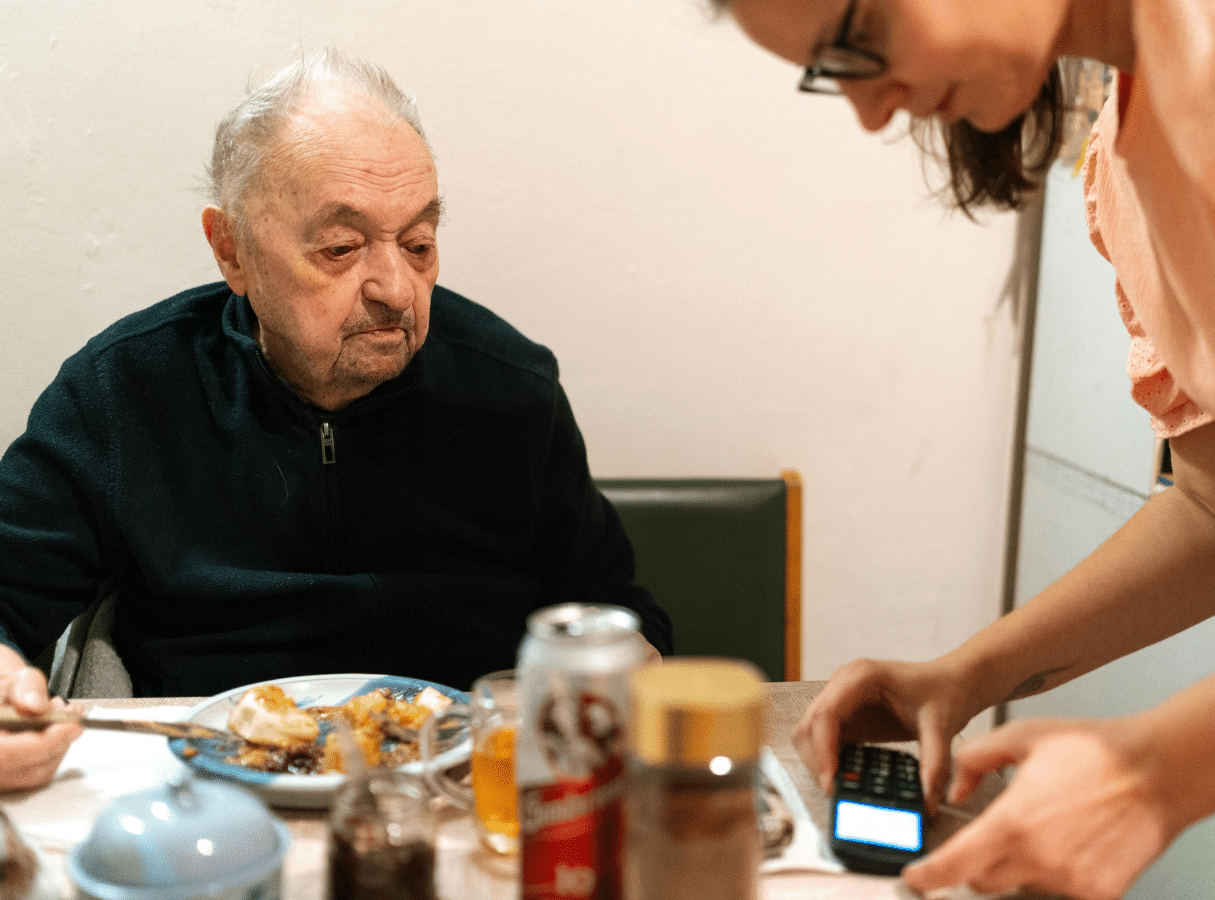
- Creating a pleasant dining environment to stimulate the appetite
- Providing feeding assistance when necessary
- Using appetite stimulants when medically appropriate
All interventions should aim to restore balance, support health goals, and align with the care recipient’s personal preferences. A well-developed nursing care plan for nutrition imbalance, less than body requirements, improves physical outcomes and supports emotional wellness.
Facilities often rely on tailored dietary programs to ensure residents meet daily nutrient goals, reduce health risks, and recover from any prior deficiencies.
Developing Care Plans Tailored to Individual Needs
A generic care plan won’t do. Instead, focus on imbalanced nutrition related to personal health history, food tolerance, and social factors. By working closely with dietitians, nursing staff can build a plan that suits individual caloric and nutritional needs without sacrificing meal enjoyment.
Developing an imbalanced nutrition nursing care plan involves:
- Performing individualized nutrition assessments
- Documenting food and fluid intake
- Monitoring weight trends and lab values
- Collaborating with the interdisciplinary team
- Evaluating effectiveness and updating regularly
Each resident has different challenges, from mobility to mental health. A well-structured plan should address each one. This article on nutrition for older adults is a helpful resource for identifying how diet impacts longevity and well-being.
Real-World Applications: NestBeyond’s Approach
At NestBeyond, we approach every case of nutritional imbalance with care, expertise, and empathy. Our team develops customized plans that include imbalanced nutrition interventions and continuous monitoring to ensure sustainable results.
We’ve found that involving family members, providing culturally appropriate meals, and fostering community dining experiences all support better nutrition and quality of life. A proactive nursing care plan for nutrition imbalance, less than body requirements, can reverse harmful trends and build a path to vibrant senior living.
If you’re working with seniors or managing a care facility, remember that each imbalanced nutrition nursing diagnosis is an opportunity to improve a life—not just a medical task. Being detailed and compassionate makes all the difference.
- Nutrition.gov for Older Adults: Federal resource for nutrition advice by age group.
- Academy of Nutrition and Dietetics – Seniors: Educational tools and updates for healthy aging and eating habits.
- NIH Senior Health: Nutrition: Guidelines on dietary supplements and their use in older adults.
Transforming Nutrition Care: A Path to Better Living
Improving nutrition in senior living isn’t a quick fix—it’s a journey. But with a focused imbalanced nutrition nursing care plan, the benefits are both immediate and long-term. You’re not just filling plates; you’re nurturing health, happiness, and hope.
Whether you’re managing imbalanced nutrition related to medical conditions, mental health, or lifestyle challenges, a clear, compassionate plan changes everything. Implementing the right imbalanced nutrition interventions will support better recovery, fewer hospital visits, and a renewed sense of dignity in aging.
For more information about how NestBeyond supports senior nutrition, or to speak with a care coordinator, call us at 866-622-4206 or email info@nestbeyond.com. Together, we can make nutrition a cornerstone of healthier aging.
Frequently Asked Questions
What are the nursing interventions for imbalanced nutrition?
Nursing interventions for imbalanced nutrition focus on improving the patient’s nutritional intake and addressing any underlying causes. Common strategies include monitoring daily food consumption, offering nutrient-dense meals, and assisting with feeding if needed. Nurses also educate patients and families about healthy dietary habits and may coordinate with dietitians. Regular weight checks and lab monitoring help track progress.
How to write a nursing care plan on malnutrition?
To write a nursing care plan on malnutrition, start by assessing the patient’s nutritional status, medical history, and any contributing factors like illness or limited access to food. Identify a nursing diagnosis such as “Imbalanced Nutrition: Less Than Body Requirements” and set measurable goals, like weight gain or improved appetite. Plan and implement meal planning, supplements, and patient education interventions. Lastly, evaluate the outcomes and adjust the plan as needed.
What is a NANDA nursing diagnosis for poor nutrition?
A common NANDA nursing diagnosis for poor nutrition is “Imbalanced Nutrition: Less Than Body Requirements.” This diagnosis is used when a patient is not consuming enough nutrients to meet their metabolic needs. Related factors include reduced appetite, digestive issues, or socioeconomic challenges. Defining characteristics might include weight loss, muscle weakness, or poor wound healing.
What is the nursing care for a person with a nutritional deficit?
Nursing care for someone with a nutritional deficit includes comprehensive assessment and targeted interventions to restore nutritional balance. Nurses provide or assist with feeding, recommend high-calorie and high-protein meals, and ensure adequate fluid intake. They also collaborate with dietitians to develop individualized meal plans. Ongoing evaluation is essential to track weight, strength, and lab results improvements.